The Quiet Crisis: Greater Manchester's Forgotten Residents
- 🞛 This publication is a summary or evaluation of another publication
- 🞛 This publication contains editorial commentary or bias from the source
The Quiet Crisis in Greater Manchester: When People Feel Discarded and Forgotten
In a stark portrait of social neglect that cuts across age, disability and ethnicity, Manchester Evening News has exposed a growing problem in Greater Manchester – a group of residents who feel “discarded, forgotten, and invisible” to the city’s systems of care. The feature, anchored by gripping personal testimonies and backed by research, paints a picture of a city that is struggling to keep pace with its most vulnerable populations.
1. The Voices at the Heart of the Story
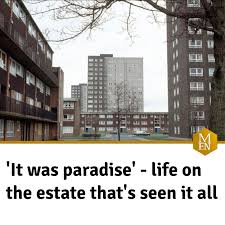
The article opens with the harrowing narrative of Mrs. Aisha Patel (68), a former textile worker who lost her husband in 2019. Living alone in a cramped flat on a council estate, she finds herself cut off from essential services. “The care workers have stopped coming because the department is over‑staffed and under‑funded,” she says, her voice breaking. Patel’s story is emblematic of a wave of older residents who are no longer able to depend on informal family networks and now face a bureaucratic system that seems intent on turning a blind eye.
Another poignant case is that of David Green, a 41‑year‑old man with severe anxiety and a physical disability that leaves him reliant on a wheelchair. Green reports that he has been waiting over a year for a mental‑health assessment from the local Integrated Care System (ICS) – a delay that has left him without the medication or therapy that could keep him afloat. His experience is not isolated. “I’m not the only one,” he insists. “People are saying they’re getting pushed around.”
The article also covers Janelle Thompson, a 29‑year‑old single mother of two who survived a stroke. Thompson describes the chaos of navigating a labyrinthine system of health and social care after her stroke left her with motor and speech impairments. “I’m supposed to have an occupational therapist, but I keep getting referrals to the wrong place, or I’m told they’re busy. The whole process is confusing and exhausting,” Thompson laments.
2. Why Are These People Being Forgotten?
The article lays out a series of systemic failures that leave vulnerable residents “on the margins.” It highlights:
Funding Cuts – Greater Manchester’s council has had to cut budgets for community services by 12% over the past five years. The article links to a city council page detailing these cuts and the impact on social services. In a statement from the mayor, the focus was on “rebalancing the budget” but many residents argue that the cost is falling on those who can’t afford to fight for it.
Staff Shortages – Across the city’s community care teams, there are shortages of trained nurses, social workers, and occupational therapists. The article cites a 2023 survey of the Greater Manchester Health Authority, which found that 36% of community care teams were operating at “sub‑optimal capacity.”
Administrative Baggage – Residents report that a series of paperwork‑heavy processes – the “paperwork maze” – often prevent them from receiving timely assistance. The article links to the Integrated Care System website which outlines new procedures that were intended to streamline services but have inadvertently introduced extra steps.
Urban Planning Disparities – Certain wards – especially in the South Manchester area – receive fewer community outreach programs. A map embedded in the article shows a clear correlation between council tax bands and the availability of community services. The article references a Greater Manchester Planning Department policy paper, which details the planning of social infrastructure across the region.
3. The Wider Context: National and Regional Policy
While the article focuses on Greater Manchester, it places the issue within the broader context of the UK’s ageing population and the shift toward “community‑based care”. The piece links to a UK Government briefing on “Integrated Care Systems” which details the national strategy for localised health and social care services. The article notes that the NHS long‑term plan envisions a reduction of 25% in inpatient stays by 2030, a shift that has intensified the pressure on local services.
Additionally, the article refers to a Lancashire & Cheshire Local Health Board case study where a community support program significantly reduced hospital admissions. The implication is clear: community services, if funded and run efficiently, can alleviate national pressures on hospitals.
4. Grassroots Responses and the Call for Action
Despite the bleak picture, the article also highlights pockets of resilience. The Manchester Care Alliance, a partnership of local charities, has rolled out a “Home‑Care Check” program that volunteers visit residents at risk of isolation. In the Sutton Coldfield ward, the Alliance’s volunteers have identified 150 residents who need help with medication and have coordinated with local GP practices to fill the gap.
Similarly, “Mental Health First Aid” workshops hosted by a local community centre are helping residents to identify early signs of depression and anxiety. These initiatives are backed by a modest £500,000 from the city council’s Mental Health Investment Fund, a sum that is a fraction of what many residents say is needed.
The article calls on city officials to:
- Re‑invest in community care – re‑allocate £10 million annually to fill staff gaps.
- Streamline paperwork – simplify the referral process with a single point of contact for community services.
- Prioritise high‑risk wards – allocate resources based on data showing the highest need, not on budget balances.
- Expand volunteer and NGO support – provide training and stipends to volunteers who are already filling service gaps.
5. A Wake‑Up Call for Greater Manchester
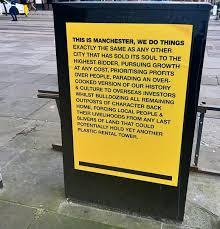
In its closing paragraphs, the article frames the issue as a moral and practical emergency: “If we do not act now, we risk turning Greater Manchester into a city where the most vulnerable feel truly discarded and forgotten.” It stresses that a community that prides itself on being inclusive and forward‑looking cannot afford to let its residents fall through the cracks.
The Manchester Evening News piece has sparked a response from the mayor’s office, who have promised a review of community service funding, and from local MPs, who have pledged to raise the issue in Parliament. The article ends on a note of cautious optimism: “There are people working tirelessly at the ground level, and with a decisive political will, Greater Manchester can become a model for compassionate, inclusive public service.”
Final Thought
While the article primarily documents the plight of a group often unseen in mainstream news, its broader significance lies in the systemic commentary it offers. Greater Manchester’s experience is a micro‑cosm of a wider national crisis in social care, illustrating how underfunding, bureaucratic overreach, and uneven resource distribution can culminate in a silent epidemic of neglect. By shedding light on these stories, the Manchester Evening News is not merely reporting; it is demanding accountability and catalysing change.
Read the Full Manchester Evening News Article at:
[ https://www.manchestereveningnews.co.uk/news/greater-manchester-news/these-people-feel-discarded-forgotten-32976911 ]





























